In this article, you will be diving into the fascinating world of healthcare policy and its profound impact on the resilience of healthcare systems. We will explore how the decisions made at a policy level can shape the ability of healthcare systems to withstand and adapt to various challenges and crises. By understanding this connection between policy and resilience, we can gain valuable insights into the strategies needed to build robust healthcare systems that can effectively respond to the ever-evolving healthcare landscape. So, grab a cup of tea and get ready to embark on this enlightening exploration together!
Definition of Healthcare Policy
Understanding healthcare policy
Healthcare policy refers to a set of guidelines, rules, and regulations formulated by governments, organizations, or institutions to guide the delivery, organization, and financing of healthcare services. These policies are designed to address various aspects of healthcare, from access and affordability to quality and patient safety. Healthcare policy aims to create a framework that ensures the provision of effective, efficient, and equitable healthcare services to individuals and populations.
Goals and objectives of healthcare policy
The primary goal of healthcare policy is to improve the health outcomes and well-being of individuals and communities. It seeks to achieve this by focusing on several key objectives, including promoting healthcare access and affordability, enhancing healthcare quality and safety, reducing healthcare disparities, and ensuring the sustainability of healthcare systems. Healthcare policies also aim to address the evolving healthcare needs and challenges of a population, such as aging demographics, chronic diseases, and emerging infectious diseases.
Importance of Healthcare System Resilience
Why healthcare system resilience matters
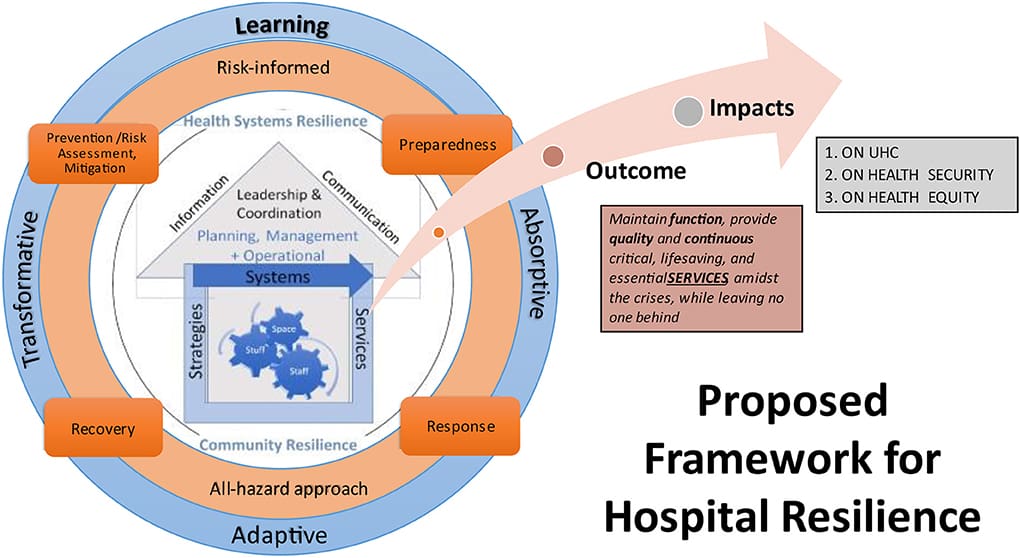
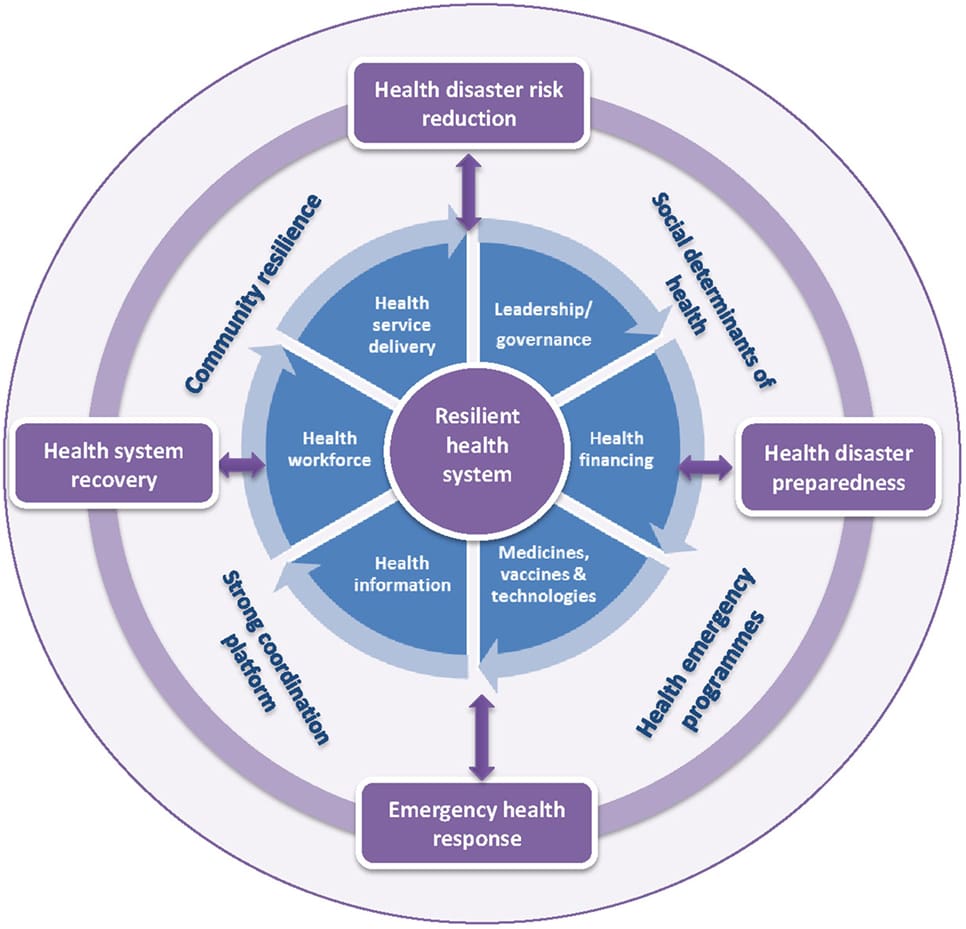
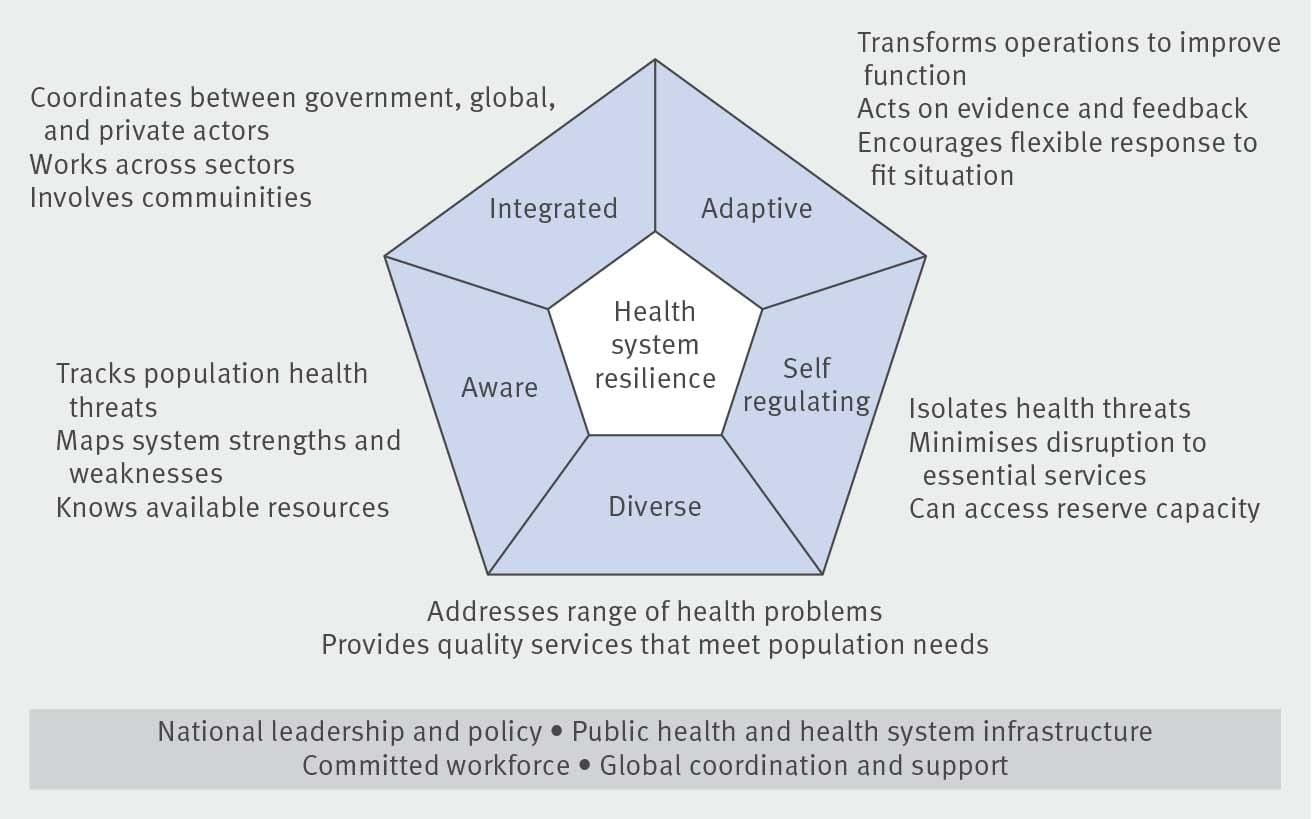
Healthcare system resilience refers to the capacity of a healthcare system to withstand and adapt to unforeseen challenges, crises, and emergencies while still delivering high-quality and accessible care. It is essential to have a resilient healthcare system as it helps ensure the continuity of healthcare services, safeguards public health, and protects vulnerable populations during times of crisis. Resilience enables healthcare systems to effectively respond to natural disasters, pandemics, terrorist attacks, or other emergencies without compromising the care provided to patients.
Ensuring continuity of healthcare services
One of the primary reasons why healthcare system resilience is crucial is to ensure the continuity of healthcare services even in the face of disruptions. Whether it is a natural disaster, a disease outbreak, or any other emergency, a resilient healthcare system can continue providing essential care to patients. This continuity is vital for both routine healthcare needs and emergencies since interruptions in healthcare services can have severe consequences for individuals’ health outcomes and overall population health.
Effective response during crises or emergencies
In times of crisis or emergencies, healthcare system resilience plays a pivotal role in ensuring an effective response. Resilient systems are better prepared to mobilize resources, coordinate efforts, and manage surge capacity during high-demand situations. This enables healthcare organizations to rapidly adapt and respond to the needs of the community, protecting public health and minimizing the impact of the emergency on individuals and populations. Healthcare policy plays a crucial role in creating the necessary frameworks and structures to enhance resilience and facilitate an effective response in such situations.
Factors Affecting Healthcare System Resilience
Infrastructure and resources
The availability and adequacy of healthcare infrastructure and resources play a significant role in determining the resilience of a healthcare system. This includes hospitals, clinics, medical equipment, medicines, and other essential resources necessary for delivering healthcare services. Sufficient infrastructure and resources help ensure the capacity to handle high patient volumes, accommodate surge capacity during emergencies, and provide necessary support for healthcare professionals to offer quality care.
Workforce and personnel
The healthcare workforce is a critical component of a resilient healthcare system. Sufficient numbers of skilled healthcare professionals, such as doctors, nurses, and allied health professionals, are essential for the continuous provision of care. Adequate staffing levels and appropriate training and development opportunities for healthcare personnel contribute to the resilience of the system. Additionally, maintaining the well-being and safety of healthcare workers is crucial in preserving the system’s resilience.
Technological advancements
Advancements in healthcare technology can significantly impact the resilience of healthcare systems. The integration of electronic health records, telemedicine, and other digital health solutions enhance the efficiency and effectiveness of healthcare delivery. These technological advancements improve communication, coordination, and the ability to exchange healthcare information, facilitating seamless care. Investing in innovative technologies strengthens the resilience of the system and enhances its ability to adapt to evolving healthcare needs and challenges.
Access to healthcare services
Access to healthcare services is a critical factor influencing the resilience of a healthcare system. Adequate access ensures that individuals can receive timely and appropriate care, regardless of their location or socio-economic status. This includes both physical access to healthcare facilities and services and financial access, ensuring that healthcare is affordable and not a barrier to receiving necessary care. Policies that improve access to healthcare, particularly for vulnerable and underserved populations, contribute to the resilience of the healthcare system.
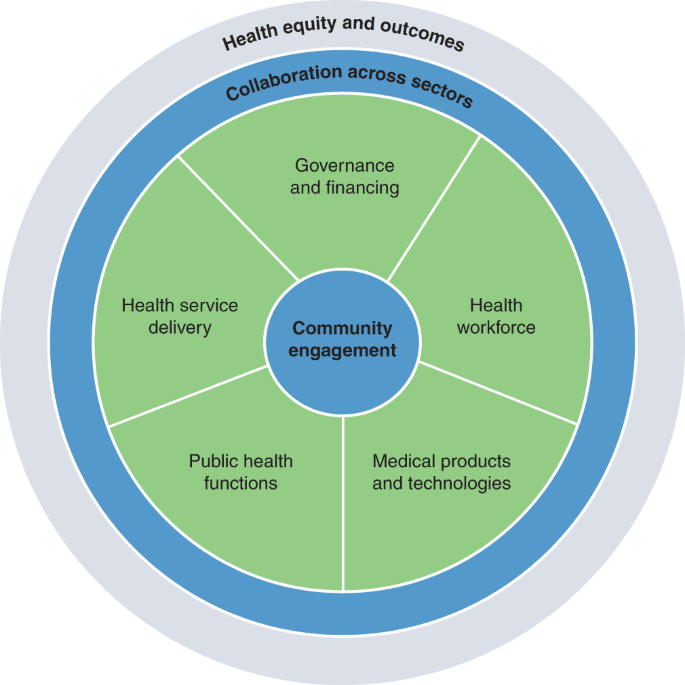
Collaboration and coordination between healthcare organizations
Effective collaboration and coordination between healthcare organizations are essential for healthcare system resilience. This includes partnerships between hospitals, primary care providers, public health agencies, emergency management teams, and other stakeholders involved in the delivery of healthcare services. Collaboration enables the sharing of resources, expertise, and information, allowing for a more coordinated and efficient response during emergencies. Healthcare policy can encourage and facilitate such collaboration through the development of networks and frameworks that promote integration and coordination.
Role of Healthcare Policy in Enhancing Resilience
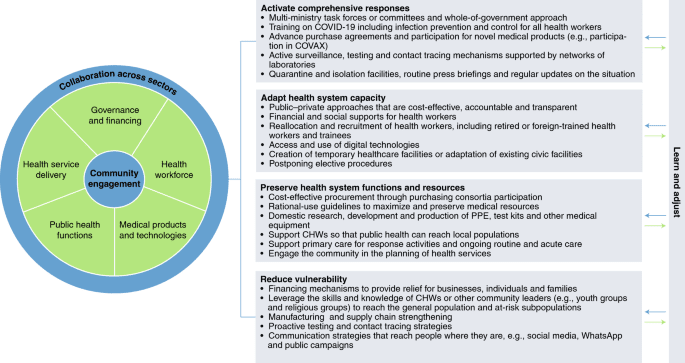
Developing comprehensive healthcare policies
One of the primary roles of healthcare policy in enhancing resilience is the development of comprehensive policies that address the various dimensions of healthcare system resilience. Policies should encompass all aspects, from infrastructure and resources to workforce development, technology adoption, and access to care. By developing comprehensive policies, governments and organizations can provide a clear direction and framework for healthcare system resilience initiatives.
Allocating resources for resilience-building initiatives
Healthcare policy plays a crucial role in ensuring the allocation of resources for resilience-building initiatives. This involves budgeting and strategic planning to allocate the necessary funding and resources to improve the resilience of healthcare systems. Adequate investment in infrastructure, workforce development, technology, and access to care is essential to build a resilient healthcare system. Healthcare policy can provide the necessary guidance and mechanisms to allocate these resources effectively and efficiently.
Ensuring healthcare policy alignment with national priorities
It is essential for healthcare policies to align with national priorities to enhance resilience effectively. By considering the unique healthcare needs and challenges of each country or region, policies can address specific vulnerabilities and strengthen areas of weakness. Healthcare policies should be in line with broader public health goals, disaster management strategies, and societal values to ensure a cohesive and coordinated approach to resilience-building efforts.
Monitoring and evaluating policy effectiveness
Healthcare policy also has a role in monitoring and evaluating the effectiveness of resilience-building initiatives. Regular evaluation of policies, programs, and interventions is necessary to assess their impact on healthcare system resilience. By collecting and analyzing data, policymakers can identify strengths, weaknesses, and areas for improvement. Evaluation allows for evidence-based decision-making and the refinement of policies to ensure they remain effective and responsive to evolving healthcare needs.
Case Studies on Healthcare Policy Impact
Examining healthcare policy impact in different countries
Analyzing the impact of healthcare policies in different countries provides valuable insights into the effectiveness of specific approaches to enhancing healthcare system resilience. Case studies can shed light on policy successes, challenges, and lessons learned. For example, countries that have successfully implemented universal healthcare policies often demonstrate improved resilience through increased healthcare access and more robust emergency response systems.
Lessons learned from successful policy implementation
Studying successful policy implementation can help identify key lessons for enhancing healthcare system resilience. Successful policies often involve strong leadership, stakeholder engagement, and effective communication strategies. Case studies can highlight innovative approaches, best practices, and potential pitfalls to avoid, informing the development and implementation of healthcare policies in other contexts.
Challenges faced in policy implementation
Understanding the challenges faced in policy implementation is equally important in enhancing healthcare system resilience. These challenges can range from political and financial constraints to human resource shortages and systemic barriers. By studying the barriers and obstacles faced in policy implementation, policymakers can develop strategies to overcome them and ensure the successful implementation of resilience-building initiatives.
Influence of Political Factors on Healthcare Policy
Political ideologies and healthcare policy
Political ideologies play a significant role in shaping healthcare policy. Different ideologies can lead to varying approaches to healthcare, such as differing opinions on the role of government in healthcare, the level of privatization, and the emphasis on individual responsibility versus collective well-being. These ideological differences influence the development, implementation, and sustainability of healthcare policies, potentially impacting healthcare system resilience.
Role of government in shaping healthcare policy
Governments play a crucial role in shaping healthcare policy, as they are responsible for creating and implementing policies that govern healthcare delivery and financing. Governments can enact legislation, establish regulatory frameworks, and allocate resources to support resilience-building efforts. The level of government involvement, the degree of centralization or decentralization, and the political priorities of the government influence the direction and effectiveness of healthcare policies.
Impact of political stability or instability on policy implementation
Political stability or instability can significantly impact policy implementation and consequently influence healthcare system resilience. Stable political environments provide a conducive setting for long-term policy planning, implementation, and evaluation. In contrast, unstable political situations, such as frequent changes in government or civil unrest, can disrupt policy continuity and hinder resilience-building efforts. Consistent political leadership and stability are essential for effective and sustainable healthcare policies.
Understanding Healthcare Policy Implementation Process
Stages of healthcare policy implementation
Healthcare policy implementation typically involves several stages. These stages can include policy formulation, policy adoption, policy implementation, and policy evaluation. Each stage requires careful planning, stakeholder engagement, and effective communication. Policymakers must consider the specific needs and context of their healthcare system during each stage to ensure successful policy implementation.
Engaging stakeholders in the implementation process
Effective policy implementation necessitates engaging a wide range of stakeholders, including healthcare professionals, administrators, policymakers, patients, and community organizations. Engaging stakeholders early in the policy implementation process fosters collaboration, ensures alignment with stakeholder needs and concerns, and improves the likelihood of successful implementation. Stakeholder involvement also promotes accountability and transparency, enhancing the overall effectiveness and resilience of the healthcare system.
Identifying barriers and facilitators for policy implementation
Identifying barriers and facilitators for policy implementation is crucial for overcoming challenges and maximizing the chances of successful implementation. Barriers can include resistance to change, lack of resources, limited capacity, and conflicting priorities. Understanding these barriers and developing strategies to address them can help overcome implementation challenges. In contrast, facilitators, such as supportive leadership, adequate resources, and effective communication, can enhance the implementation process and contribute to healthcare system resilience.
Addressing challenges in policy implementation
Challenges in policy implementation are common and should be anticipated and addressed proactively. Healthcare policy implementation often requires overcoming bureaucratic hurdles, managing resistance to change, and navigating complex healthcare systems. Strategies for addressing these challenges include effective communication and education, targeted training and capacity-building initiatives, and ongoing monitoring and evaluation to identify and mitigate barriers to successful implementation.
Evaluating the Effectiveness of Healthcare Policies
Measuring resilience outcomes
Evaluating the effectiveness of healthcare policies involves measuring resilience outcomes. Resilience indicators can include measures of access to care, healthcare quality and safety, healthcare workforce capacity, and the ability to respond to emergencies. By collecting and analyzing data on these indicators, policymakers can assess the impact of policies on healthcare system resilience. Measuring resilience outcomes allows for evidence-based decision-making and the identification of areas for improvement.
Assessing policy impact on healthcare system performance
Assessing the impact of healthcare policies on the performance of healthcare systems is vital in determining their effectiveness. This involves examining key performance indicators, such as healthcare utilization rates, patient satisfaction, healthcare costs, and health outcomes. By evaluating these performance measures, policymakers can gauge the extent to which policies have improved healthcare system resilience and contributed to the overall well-being of the population.
Using data and metrics to evaluate policy effectiveness
Data and metrics are essential for evaluating policy effectiveness. The collection and analysis of data related to healthcare utilization, health outcomes, and financial indicators provide valuable insights into the impact of policies on healthcare system resilience. Generating meaningful metrics and utilizing robust data collection methods allows policymakers to make informed decisions, identify trends, and monitor the effectiveness of policies over time. Regular evaluation using data and metrics ensures that policies remain relevant and responsive to the evolving needs of the healthcare system.
Recommendations for Enhancing Healthcare System Resilience
Promoting interdisciplinary collaboration
Enhancing healthcare system resilience requires interdisciplinary collaboration between various stakeholders. By promoting collaboration between healthcare providers, public health agencies, emergency management teams, and community organizations, policymakers can strengthen the collective ability to respond to crises and emergencies. Interdisciplinary collaboration facilitates resource sharing, coordination of efforts, and the development of comprehensive strategies to enhance resilience.
Increasing investment in healthcare infrastructure
Investing in healthcare infrastructure is crucial for enhancing system resilience. Allocating resources for the construction, maintenance, and upgrading of healthcare facilities ensures their suitability to handle emergencies and adequately accommodate patient needs. Upgrading and modernizing medical equipment and technologies also contribute to the resilience of the healthcare system. Increased investment in infrastructure strengthens the capacity to deliver quality care during normal operations and effectively respond during crises.
Prioritizing workforce development and training
Developing and retaining a skilled healthcare workforce is essential for enhancing system resilience. By prioritizing workforce development and training, policymakers can ensure that healthcare professionals have the necessary skills and knowledge to respond to emergencies effectively. Offering ongoing training opportunities, supporting professional development, and implementing innovative workforce models, such as task-shifting and telehealth, can contribute to workforce resilience and improve overall system readiness.
Fostering innovation and technology adoption
Innovation and technology play a crucial role in enhancing healthcare system resilience. Policymakers should promote the adoption of digital health solutions, telemedicine, and other innovative technologies to improve access, communication, and coordination in healthcare delivery. Supporting research and development in healthcare technology creates opportunities for innovation and fosters greater system preparedness and resilience.
Ensuring equitable access to healthcare services
Equitable access to healthcare services is a fundamental aspect of healthcare system resilience. Policymakers should prioritize policies that address health disparities and ensure that underserved populations have access to timely and appropriate care. This includes improving access to primary care, addressing social determinants of health, and implementing strategies to reduce barriers to care, such as geographical distance, cultural or language barriers, and financial constraints. By focusing on equity, policymakers can enhance overall system resilience and improve health outcomes for all individuals.
Conclusion
In conclusion, healthcare policy plays a critical role in enhancing healthcare system resilience. By understanding healthcare policy, its goals, and objectives, we can appreciate its importance in ensuring the continuity of healthcare services and effective response during crises. Factors such as infrastructure, workforce, technology, access, and collaboration significantly influence healthcare system resilience, and healthcare policy plays a crucial role in addressing these factors. Through the development of comprehensive policies, resource allocation, and monitoring, healthcare policies can enhance resilience and contribute to improved health outcomes. By examining case studies, understanding the influence of political factors, and evaluating policy effectiveness, we can learn valuable lessons and make informed recommendations for enhancing healthcare system resilience. Ultimately, continuous policy evaluation and adaptation are essential to ensuring the ongoing effectiveness and relevance of healthcare policies in promoting resilience and protecting the health and well-being of individuals and communities.